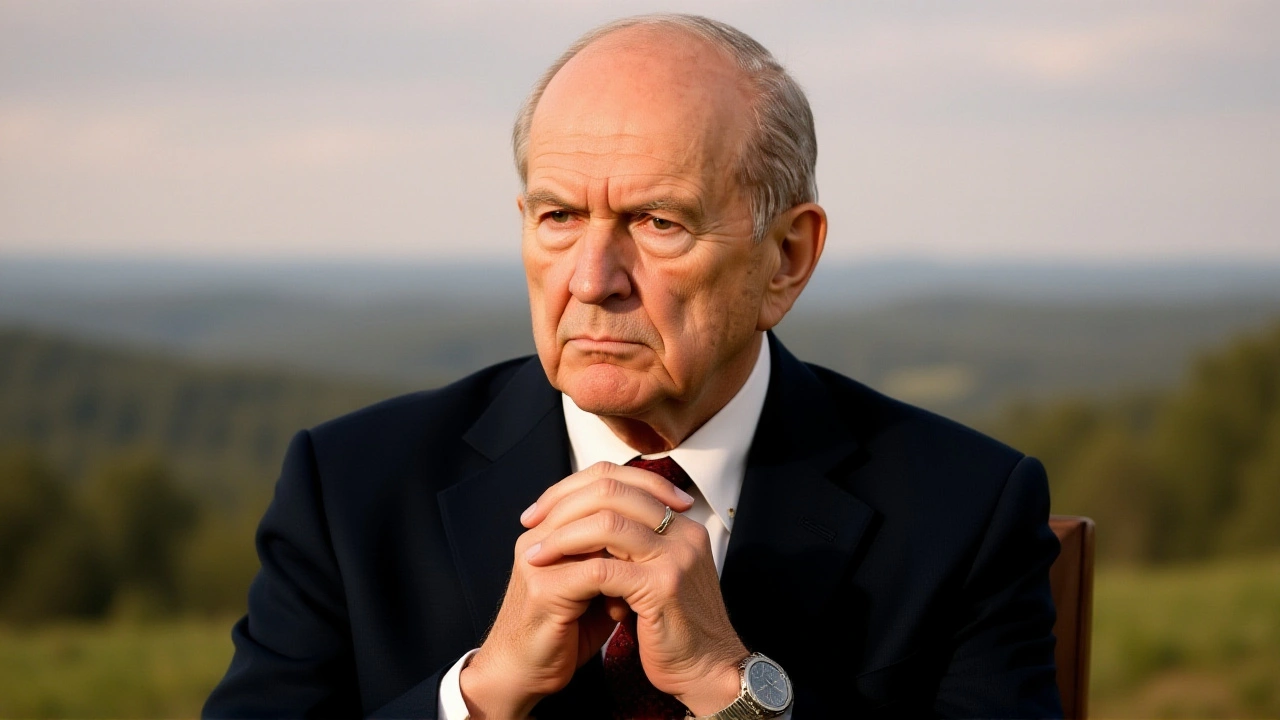
When Senator Jerry Moran helped shepherd the One Big Beautiful Bill Act (OBBBA) through Congress, few imagined the ripple it would send through the Sunflower State’s health system. The legislation, signed on July 4, 2025, used a fast‑track budget reconciliation process to redirect more than $4 trillion in federal spending, slashing taxes while reshaping Medicaid rules that affect KanCare, Kansas’s combined Medicaid and CHIP program.
Kansas, home to roughly 29 million people, saw its Federal Medical Assistance Percentage (FMAP) sit at 61.87% for Medicaid and 73.31% for CHIP in fiscal year 2025. In plain English, for every dollar Kansas spends on Medicaid, the federal government chimes in with about $1.62. The state’s KanCare program currently covers about 440,000 low‑income residents – from children and pregnant women to seniors and people with disabilities – making it the second‑largest line item in the state budget after K‑12 education.
Historical Context: Medicaid in Kansas Before the OBBBA
For decades, Kansas relied on a patchwork of state‑run agencies to administer Medicaid. The Kansas Department of Health and Environment partnered with the Kansas Department for Aging and Disability Services to oversee eligibility, while managed‑care organizations handled day‑to‑day service delivery. This structure kept the program afloat but left rural hospitals scrambling for reimbursements, especially as enrollment grew.
Rural health woes weren’t new. A 2023 CHQPR study warned that roughly 29% of rural hospitals across Kansas and neighboring states faced imminent closure within three years. The underlying causes – low patient volumes, staffing shortages, and thin margins – pre‑dated any federal policy shift.
Medicaid Reform Under the One Big Beautiful Bill Act
OBBBA’s Medicaid provisions aim to tighten eligibility and shift more cost‑sharing onto states. While the FMAP rate remains unchanged for 2025, the law mandates that late eligibility reviews be treated as new applications starting July 1, 2025. Beneficiaries now must answer “yes” to prior medical expense questions to qualify for retroactive coverage.
Administrative tech also takes a hit. Provider Electronic Solutions (PES) will no longer be supported by the Kansas Medical Assistance Program (KMAP) after October 14, 2025. All providers must route electronic data interchange (EDI) transactions through the newer Kansas Medicaid Management System (KMMS), a move many smaller rural clinics fear will strain limited IT resources.
On the enrollment front, the health insurance marketplace opens November 1, 2025, and runs through January 15, 2026, with coverage effective January 1, 2026, for anyone who signs up before December 15. This window is critical for millions who have been on the margins of coverage for years.
Rural Health Transformation (RHT) Program: A $50 B Federal Push
In late September 2025, Kansas filed an application for the brand‑new Rural Health Transformation Program, a $50 billion initiative embedded in the OBBBA. The program, administered by the Centers for Medicare and Medicaid Services, requires each state to submit a detailed transformation plan by the end of 2025.
According to Governor Laura Kelly, the state’s plan was crafted in collaboration with the University of Kansas Health System Care Collaborative. A webinar on September 29, 2025, gave stakeholders a glimpse of the application and answered questions about the upcoming funding pipeline.
The RHT fund will pour roughly $1 billion into Kansas over the next five years – about $200 million per year – with the first $25 billion distributed equally among all states that submit a successful application. The remaining $25 billion will be allocated at CMS’s discretion, based on demonstrated need and project viability.
“Throughout the reconciliation process, I worked with my colleagues to establish $50 billion in funding for the Rural Health Transformation Program,” said Senator Jerry Moran. “With Kansas estimated to receive approximately $1 billion, I look forward to working with the state government and the University of Kansas Health System Care Collaborative to ensure our rural providers get the resources they need.”
Stakeholder Reactions: Hope, Skepticism, and Calls for Clarity
Cindy Samuelson, spokesperson for the Kansas Hospital Association, was cautiously optimistic. “There’s still a lot to figure out with that Rural Health Transformation Fund. Don’t get me wrong – Kansas hospitals appreciate any support, but this would only be temporary and it’s not yet clear who would benefit,” she said.
Across the border, Rich Rasmussen, president and CEO of the Oklahoma Hospital Association, dismissed the federal cash as a “drop in the bucket,” noting that the cuts driven by the OBBBA’s broader spending overhaul far outweigh the $200 million Kansas expects each year.
Healthcare researchers echoed those concerns, pointing out that without systemic reforms to reimbursement rates and workforce pipelines, a $1 billion injection may merely postpone inevitable closures.
Implementation Challenges and What Comes Next
The RHT plan must outline concrete steps: upgrading telehealth infrastructure, expanding broadband in underserved counties, and creating incentive packages to retain physicians. The Kansas Rural Health Innovation Alliance – a newly formed coalition of providers, insurers, and community groups – has been tasked with tracking progress and reporting back to CMS.
Meanwhile, the Kansas Department of Health and Environment is scrambling to train staff on the new KMMS system before the October 14 deadline. Small clinics fear that the learning curve could translate into delayed claims, potentially worsening cash‑flow problems.
Looking ahead, the state will need to submit annual performance reports to CMS. If the pilot projects demonstrate measurable improvements – such as a 10% reduction in emergency‑room visits or a 15% increase in primary‑care appointments in rural zip codes – additional funding could be earmarked for expansion.
Background Deep Dive: Federal Reconciliation and Its Ripple Effects
The OBBBA, formally known as H.R. 1, was championed by a coalition of Republican and some moderate Democrats as a budget‑saving vehicle. By invoking the budget reconciliation process, lawmakers circumvented the usual 60‑vote Senate threshold, pushing through a package that combined $4 trillion in tax cuts with targeted spending on border security, defense, and energy. Medicaid reform, though only a portion of the bill, was highlighted as a “safety‑net realignment” – a euphemism for shifting more responsibility onto states.
Critics argued that the rapid passage left little room for stakeholder input, especially from vulnerable populations dependent on Medicaid. In Kansas, the timing coincided with rising concerns about the sustainability of rural hospitals, a problem exacerbated by the pandemic’s lingering financial scars.
Nonetheless, the inclusion of the Rural Health Transformation Program signaled a recognition that rural health cannot be addressed solely through block‑grant cuts. By earmarking $50 billion for a five‑year effort, Congress aimed to create a parallel track of investment – albeit one that requires states to demonstrate clear, outcome‑based plans.
Whether Kansas can convert that promise into lasting improvements remains to be seen. The next few months will test the state’s ability to navigate new administrative systems, secure the RHT funding, and keep its 440,000 KanCare members covered amid shifting federal rules.
Frequently Asked Questions
How will the Rural Health Transformation Fund affect Kansas’s rural hospitals?
The fund allocates about $200 million per year to Kansas, earmarked for projects like telehealth expansion, broadband upgrades, and provider recruitment incentives. While the money can help modernize facilities, experts warn it may not fully offset the deeper financial cuts imposed by the OBBBA, so many hospitals could still face closure without additional state support.
What changes are Kansas Medicaid beneficiaries seeing after the OBBBA?
Beneficiaries must now treat late eligibility reviews as new applications and answer detailed questions about prior medical expenses to receive retroactive coverage. The state also discontinued Provider Electronic Solutions, forcing providers to submit claims through the KMMS platform starting October 14, 2025.
When can Kansans enroll in the health insurance marketplace?
Open enrollment runs from November 1, 2025, through January 15, 2026. Coverage becomes effective on January 1, 2026, for anyone who signs up before December 15, 2025. This window is crucial for those whose Medicaid eligibility lapsed under the new rules.
Why are some lawmakers and hospital leaders skeptical about the RHT funding?
Critics point out that the $1 billion Kansas expects over five years is modest compared with the scale of Medicaid cuts and the chronic underfunding of rural health infrastructure. Without clear criteria for fund distribution, there’s a risk that only a handful of larger systems will benefit, leaving smaller hospitals “in the cold.”
What role does the Kansas Rural Health Innovation Alliance play?
The Alliance, formed after the September 26, 2025 application, coordinates stakeholder input, tracks progress on the RHT plan, and serves as the primary liaison between state agencies and CMS. Its goal is to ensure that funding requests align with on‑the‑ground needs of rural providers.


When I think about the recent shifts in Kansas health policy, the first thing that strikes me is the sheer scale of the federal money involved. The $50 billion Rural Health Transformation Program is a number that can barely fit on a coffee cup, yet it is spread thin across dozens of states. Kansas, with its $1 billion share, will see roughly $200 million a year, which sounds generous until you remember the chronic under‑funding of rural hospitals. Those facilities have been running on razor‑thin margins for years, and a few hundred million dollars hardly patches a gaping wound. Moreover, the new Kansas Medicaid Management System replaces the old Provider Electronic Solutions, forcing small clinics to scramble for IT support. That transition alone can cause delayed claims, which translates directly into cash‑flow crises for the most vulnerable providers. The OBBBA also tightens eligibility, meaning many who were previously covered now have to re‑apply, adding administrative overhead that the state health departments are not prepared for. Rural communities already suffer from provider shortages, and without a clear pipeline for new doctors, the funding will only be a Band‑Aid. The telehealth upgrades sound promising, but broadband in remote Kansas counties is still a myth for many residents. The Kansas Rural Health Innovation Alliance is tasked with tracking progress, yet it is unclear how much authority it truly has over state agencies. If the performance metrics focus solely on reduced ER visits, providers might cut needed services just to meet targets. The potential for perverse incentives is high, and the federal oversight may not catch every slip. In the end, the $1 billion may keep a few hospitals afloat while the rest inch closer to closure. The timing of the new enrollment window adds another layer of complexity for those who missed the deadline. It is a perfect storm of policy change, funding uncertainty, and on‑the‑ground reality. Only a coordinated effort that addresses reimbursement rates, workforce training, and true broadband expansion can turn this fleeting cash infusion into lasting change.
Reading about the OBBBA’s impact on Kansas makes me feel a deep pang of frustration for our nation’s health system, especially when so much money is being tossed around like confetti at a parade. It is hard not to see this as yet another example of Washington’s grand promises that never translate into real improvements for the common folk. Rural hospitals are the lifeblood of small towns, and the federal plan, while sizable on paper, feels like a token gesture when you compare it to the massive cuts that are also part of the bill. The new Medicaid eligibility hurdles will push even more families into uncertainty, and the bureaucratic maze that follows is bound to stall care. I cannot help but wonder how many of these initiatives are truly designed for the people versus being political theater. The rush to replace the Provider Electronic Solutions with the KMMS platform is a clear sign that the system is being forced to adapt without proper resources. While some may point to the telehealth expansions as a silver lining, without reliable broadband the promise evaporates. The rhetoric about “transforming” rural health is sweet, but the substance is still missing. In my view, the federal government should focus more on protecting existing services than on creating new, perhaps unnecessary, reporting structures.
Totally feel you on that 🙌. The funding sounds good, but the rollout feels like a maze. Let’s hope the Alliance can actually streamline things 😊. Fingers crossed for the clinics!
The plan does lay out specific goals, such as reducing emergency visits by ten percent. That’s a concrete target that can be measured. If the state follows through with the broadband upgrades, we might see real benefits. It will take patience and coordination across agencies.
Honestly, the whole thing feels like a corporate buzzword fest. They talk big but deliver small, and many rural docs will just shrug it off. The miss‑match between ambition and budget is glaring. If they dont get the details right, it’s all just hype.
Oh great, another federal grant to save the dying hospitals. Because that’s never worked before. Let’s see how long the money lasts before the next budget cut.
At least this time they mentioned telehealth. Maybe that’ll keep some doors open, but I doubt it will stop the inevitable closures. The paperwork alone could choke smaller practices.
It is essential that the state’s application to the Rural Health Transformation Program demonstrates measurable outcomes. The inclusion of specific metrics, such as a fifteen‑percent increase in primary‑care appointments, will strengthen the case for additional funding. Coordination with the University of Kansas Health System Care Collaborative provides a solid foundation. Moreover, a transparent reporting mechanism will foster accountability. I am optimistic that with diligent implementation, the intended improvements can be realized.
Indeed;;; the metrics are crucial!! However,, the timeline is tight,, and the staff training on KMMS is lagging... Need more resources...
The whole thing reads like a glossy brochure-pretty, but lacking substance. It’s a half‑baked attempt at a miracle.
True, the brochure looks nice, yet the real test is on the ground. Let’s keep an eye on how the funds are actually used.
What most people don’t see is that the OBBBA is part of a larger agenda to shift healthcare costs onto states while rewarding contractors who lobby in D.C. The $50 billion appears generous, but the allocation formula favours states with compliant leadership. Kansas, by aligning with federal priorities, may be unwittingly opening the door to even more federal oversight. The secrecy surrounding the performance metrics suggests a desire to control outcomes without public scrutiny. In the end, it’s a strategic move to weaken state autonomy over health policy.
Interesting perspective; it does raise questions about the balance of power. If the federal hand is too heavy, the state’s own solutions might be stifled. Still, perhaps there’s room for collaboration that respects local needs. Let's hope transparency improves as the program unfolds.
The discourse around rural health must transcend mere fiscal calculations and address systemic inequities. A nuanced strategy is required, not just a band‑aid of dollars.
Indeed, the complexity of rural health cannot be reduced to simple budget lines. When we examine the interplay between provider shortages, patient demographics, and geographic isolation, a multifaceted approach emerges. Telehealth, while promising, depends on robust broadband, which is still uneven across Kansas counties. Workforce development programs need incentives that are both attractive and sustainable, otherwise turnover will remain high. Moreover, community engagement plays a pivotal role; without local buy‑in, even the best‑funded initiatives may falter. The RHT program’s emphasis on measurable outcomes is a step forward, but the metrics must capture quality of care, not just volume. Ultimately, a collaborative framework that includes state, federal, and private stakeholders will be essential for lasting change.
Sometimes I wonder if policies are like rivers-ever flowing, shaping the land they touch. The OBBBA may carve new paths for Kansas, but the terrain will decide whether those paths become highways or dead ends. Let’s stay hopeful and keep the dialogue alive.
Only time will tell.